Introduction: Non-Hodgkin's lymphoma (NHL) is the most prevalent hematologic malignancy, with most people diagnosed aged over 65 years (Alexander et. al. Int.J.Cancer 2007). Older populations have more comorbid health conditions, frailty, polypharmacy, and health resource use (Ogle et. al. Cancer 2000). The complex interplay of these factors may influence the prescription of curative therapy and prognosis. In trials evaluating NHL therapies, elderly patients are underrepresented, particularly those with frailty or comorbidity, resulting in knowledge gaps. We report a retrospective, population-based cohort study of aggressive NHL patients and examine the impact of age and its interaction with comorbidity and polypharmacy on treatment patterns and survival.
Methods: Using the Manitoba Cancer Registry we identified patients aged over 18 years with NHL diagnosed from 2004-2015. We limited the cohort to aggressive NHL types using morphology codes. Data on demographics, stage, NHL type, comorbidities, polypharmacy, and chemotherapy were obtained from population-based provincial databases. Comorbidity was measured using Johns Hopkins ACG System software, which factored in all measured hospital-based and outpatient medical services utilized and collapsed them into one of six Resource Utilization Band (RUB) categories, from no use to very high user. Overall survival (OS) was calculated using Kaplan-Meier curves. Cox proportional hazards regression models were constructed to determine the interaction of age with a variety of factors. Multi-variable logistic regression was also used to examine the receipt of chemotherapy and the interaction with age.
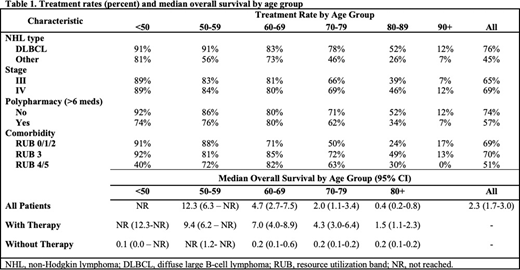
Results: In our cohort of 1,073 patients with aggressive NHL, 704 were treated with systemic chemotherapy. Treatment rates decreased with increasing age and medication count, while stage and comorbidity had little impact (Table 1). Median OS decreased with age among treated patients and was very short without chemotherapy (Table 1). Multivariate analyses found that individuals with increasing age, stage III, unknown stage, histology other than DLBCL, and higher medication counts were less likely to receive chemotherapy. For the receipt of chemotherapy, no age interactions were found. In addition, in patients who received chemotherapy, increased age and stage were associated with poorer survival, while more recent year of diagnosis improved survival. No age interactions with a substantial impact on survival were found.
Conclusions: OS in aggressive NHL diminishes with increasing age, but is longer in those receiving chemotherapy across all age groups. Comorbidity and medication count influenced the receipt of chemotherapy and OS. Higher medication count was only independently associated with less likelihood of receiving chemotherapy, while comorbidity was not independent of other factors for either receipt of chemotherapy or OS.
Dawe:AstraZeneca Canada: Research Funding; AstraZeneca Canada: Membership on an entity's Board of Directors or advisory committees; Boehringer-Ingelheim: Honoraria; Merck Canada: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.